When 75-year-old Clark Drayton, who was typically active, began experiencing fatigue and persistent weakness in his left leg, he thought his symptoms were lingering side effects of COVID-19.
“I was having less and less energy,” he says. “I became worried about driving and couldn’t do some regular activities like riding my bike.”
Clark decided to visit his primary care physician. Following a magnetic resonance imaging (MRI) scan, he received a shocking phone call instructing him to rush to the emergency room immediately. Despite experiencing only two symptoms – fatigue and left leg weakness – he was diagnosed with a brain bleed, a condition typically associated with more severe symptoms such as confusion or headaches.

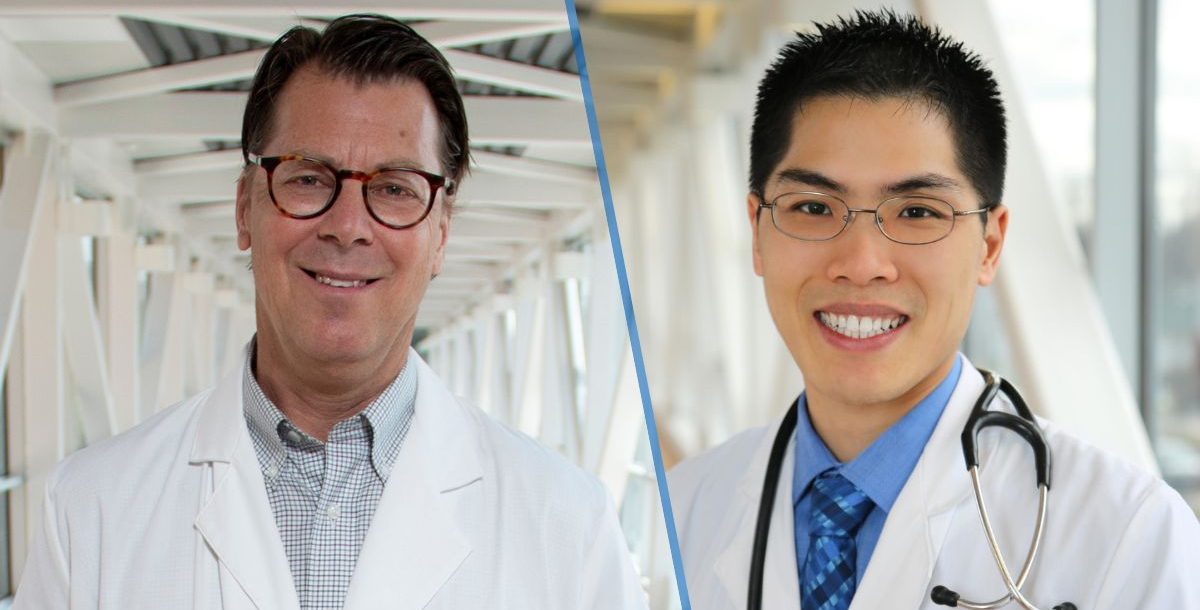
Under the care of Mercy Health neurosurgeon Brian F. Hoeflinger, MD, Clark underwent burr hole surgery to alleviate the pressure caused by the hematoma, a procedure that yielded remarkable results.
The results were life-changing.
“My left leg was dragging before surgery, and that was better almost immediately after my procedure,” he recalls. “I am so thankful for Dr. Hoeflinger and his team. They knew me personally and were really invested in my recovery.”
But Clark’s journey did not end there. The medical team explained to him that he was at risk for recurrence, which would require additional surgeries. Neuroendovascular surgeon Eugene I. Lin, MD, offered him the opportunity to participate in the MEMBRANE clinical trial, which he eagerly embraced.
“Dr. Lin explained the situation and procedure very thoroughly. He was approachable, so even though this was an overwhelming time for me, I felt very comfortable with my decision,” Clark says. “I was very grateful to have access to this treatment to help prevent additional surgeries in the future.”
During the minimally invasive procedure, the surgeon blocks the artery that supplies blood to the abnormal membranes and contributes to the persistence and growth of the subdural hematoma. The procedure has been proven to significantly reduce the chances of needing additional surgeries based on the initial results from the three trials. Moreover, the complications associated with the embolization procedure have been minimal, with no compromise to neurological function.
“We are very appreciative that Mr. Drayton chose to participate in the trial,” Dr. Lin says. “It was very exciting to hear the initial positive trial results from the three studies studying different methods at the 2024 International Stroke Conference earlier this year. Having a more effective treatment for subdural hematomas will benefit our patients as our population ages and patients are treated with anticoagulation.”
Throughout his hospital stay, Clark was deeply touched by the level of care he received.
“I felt informed and supported every step of the way. My nurses always made sure I was comfortable, and there was never a delay in care. It was quite pleasant for a hospital visit,” he says.
Discharge brought with it a flurry of follow-up appointments and imaging sessions, all seamlessly coordinated by the hospital staff. This allowed Clark to focus on his recovery and the joy of spending Christmas with his family – a true miracle after such a challenging ordeal.
Months later, as Clark reflects on his journey to recovery, he is filled with gratitude for the skilled professionals who guided him. Thanks to their expertise and unwavering dedication, he is once again able to enjoy the simple pleasures of life.
“I can go to the grocery store and up and down stairs without feeling fatigued,” he says. “I can also maintain my lawn and ride my bike outdoors. I couldn’t do those things before.”
Learn about the neurology and neurosurgery services we offer at Mercy Health.