Hearing that you need breast cancer surgery can feel overwhelming and scary. Whether you’re facing a diagnosis yourself or supporting someone who is, it’s vital to have the right information available to you.
If you’ve been diagnosed with breast cancer, need a mammogram or are at higher risk of developing breast cancer, make an appointment with your primary care provider who can refer you to the right services or specialists.
What is breast cancer surgery?
Breast cancer surgery is a primary option for most breast cancer treatment. It involves removing cancerous tissue from the breast and, in some cases, nearby lymph nodes. The goal is to eliminate as much of the cancer cells as possible and prevent it from spreading further.
There are several types of breast cancer surgery:
- Lumpectomy: Also called breast-conserving surgery, this removes only the tumor and a small margin of surrounding healthy tissue. It’s often followed by radiation therapy to reduce the risk of recurrence.
- Mastectomy: This removes all breast tissue from one or both breasts. It may be recommended for larger tumors, multiple tumors, or certain aggressive cancer types.
- Sentinel lymph node biopsy: A procedure to check if cancer has spread to nearby lymph nodes.
- Lymphadenectomy: Removal of multiple lymph nodes for further testing.
- Breast reconstruction: Optional surgery to restore the breast’s shape after cancer removal.
Why might you need breast cancer surgery?
Surgery is often the first line of defense against breast cancer. It may be recommended for:
- Early-stage breast cancer: When the tumor is localized and hasn’t spread.
- Diagnosis: To confirm cancer type and stage.
- Prevention: For those with high genetic risk (e.g., BRCA mutations).
- Symptom relief: In advanced cases, surgery may help alleviate pain or discomfort.
Your health care team will consider factors like tumor size, location, cancer type, overall health and personal preferences when recommending surgery to treat breast cancer.
Myths and facts about breast cancer surgery
Your provider will be able to provide the information you need to make an informed decision about your options regarding breast cancer surgery. Knowing the facts and being able to separate them from fiction is part of that decision process.
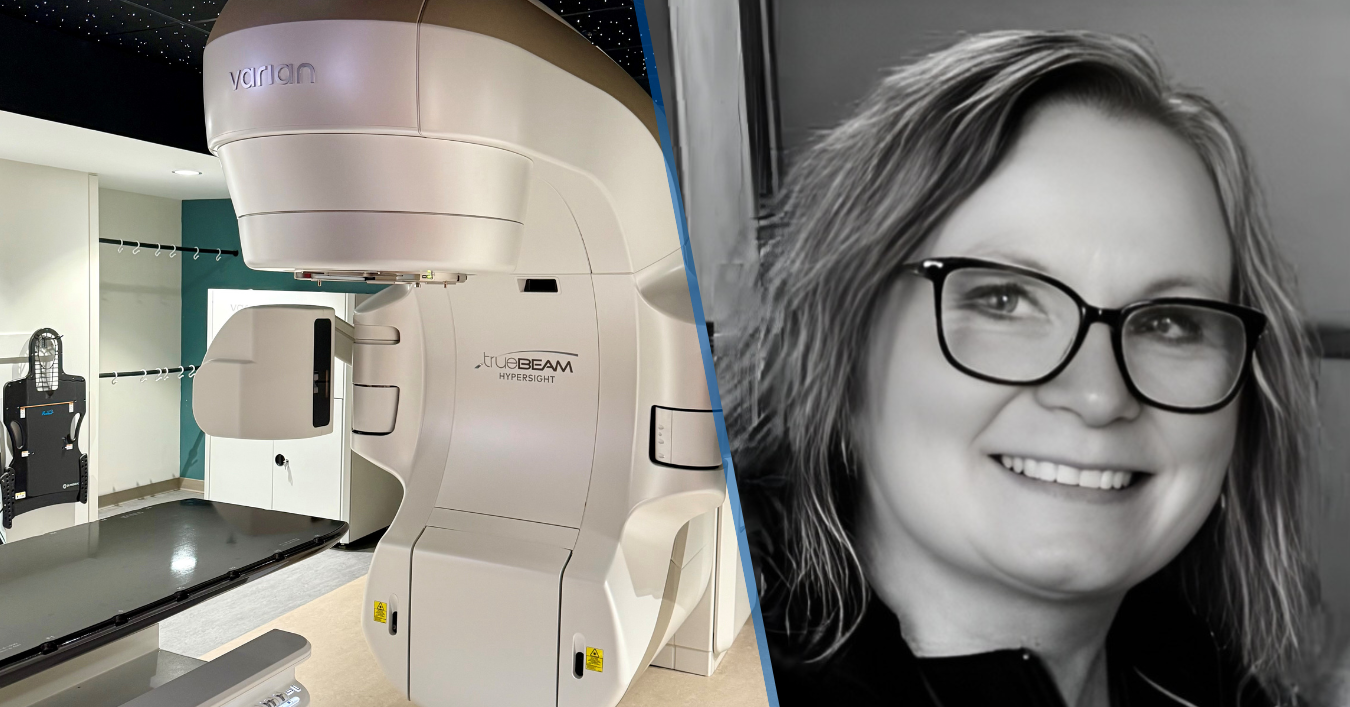
“Fear and confusion often come from misinformation,” says Colleen Alexander, MD, a breast surgeon in our Springfield market. “The more women know about their options, the more empowered they feel to make confident decisions that reflect their values and priorities.”
Myth: Surgery always means losing both breasts
Fact: Many believe a breast cancer diagnosis automatically leads to a double mastectomy.
In reality, lumpectomy is often a viable option, especially for early-stage cancers. Studies show that lumpectomy followed by radiation offers similar survival rates to mastectomy for many patients.
“A mastectomy is not automatically the better or safer option,” Dr. Alexander explains. “Treatment should be individualized.”
Myth: Surgery spreads the cancer
Fact: This myth is rooted in fear, not fact, and has been debunked. Surgery does not cause cancer to spread. In fact, removing the tumor is critical to stopping its growth. Surgeons take precautions to avoid disturbing surrounding tissues unnecessarily.
“Surgery is often the first and most important step in curing breast cancer,” Dr. Alexander says. “There’s no evidence it causes the disease to spread.”
Myth: Bras and antiperspirants cause breast cancer
Fact: Despite viral claims, there’s no scientific evidence linking bras or antiperspirants to breast cancer. These myths have been debunked by multiple studies and organizations.
Myth: You can’t have breast reconstruction after radiation
Fact: While radiation can impact planning for breast reconstruction surgery, it doesn’t rule it out.
“With advanced techniques, we can often offer successful reconstruction – even after radiation,” Dr. Alexander says. “It’s all about personalized planning.”
Myth: If your tumor is small, you don’t need surgery
Fact: Tumor size is only one part of the equation. “Even small cancers usually require surgical removal to ensure complete treatment,” Dr. Alexander adds. “Surgery helps us confirm the diagnosis and reduce the risk of recurrence.”
Myth: If your mom had breast cancer, you will too
Fact: While family history can increase risk, most people diagnosed with breast cancer do not have a close relative with the disease. Genetic testing and regular screenings are key to managing risk.
What happens before and after surgery?
Before surgery, you’ll meet with your surgeon to discuss:
- Your diagnosis and treatment options
- Potential side effects and recovery time
- Whether reconstruction is right for you
After surgery, recovery varies based on the procedure. You may experience swelling, pain or changes in breast appearance. Follow-up care often includes radiation, chemotherapy or hormone therapy depending on your cancer type and stage.
How we can help
Breast cancer surgery is a powerful tool in the fight against cancer. By understanding the facts and dispelling myths, you can make informed decisions and support others with compassion and clarity.
The breast cancer care team – surgeons, nurse navigators and support staff – is committed to helping every patient feel informed, empowered and supported. Make an appointment with your primary provider today to discuss what options are available.
Learn about the cancer care and oncology services we offer at Mercy Health.